 Norman Doidge, MD, is a psychiatrist, psychoanalyst and author of The Brain That Changes Itself .He is executive director of Health and the Greater Good.Just before Christmas, without much fanfare, Ontario became the first province to approve fluvoxamine – a decades-old drug few had heard of – for the early treatment of COVID-19.The December 20 announcement, coming at a time when Canadians were preoccupied with Omicron, and the fear hospitals would soon be overwhelmed, received hardly any news coverage.
Norman Doidge, MD, is a psychiatrist, psychoanalyst and author of The Brain That Changes Itself .He is executive director of Health and the Greater Good.Just before Christmas, without much fanfare, Ontario became the first province to approve fluvoxamine – a decades-old drug few had heard of – for the early treatment of COVID-19.The December 20 announcement, coming at a time when Canadians were preoccupied with Omicron, and the fear hospitals would soon be overwhelmed, received hardly any news coverage.
Fluvoxamine is a “repurposed drug,” and comes from what might seem like a most unlikely source – psychiatry.It is an antidepressant used most commonly to treat obsessive-compulsive disorder.
The drug has had two randomized control trials, or RCTs (the highest level of evidence) and four observational studies showing it keeps people with COVID out of hospital, from requiring intubation, and helps prevent death.The discovery of its anti-COVID properties came after impressive sleuthing in France and the United States.
Then a partnership co-led by a team of Canadians conducted the large randomized trial that proved what it could do.
This is a good news story, about our public-health officials doing something right, and showing flexibility, at a time when we are learning the limits of our vaccines and accompanying strategies.Reappraisal is in the air, driven by everyone’s two-year-experience with the pandemic – scientists included.
Philanthropist Bill Gates.Arnd Wiegmann/Reuters
Consider how things appeared in April, 2020, when Bill Gates, whose foundation is the largest private contributor to the World Health Organization, said : “The ultimate solution, the only thing that really lets us go back completely to normal and feel good … is to create a vaccine.” His “only” meant, that in practice, our chief hope and focus – in research, policy, in the media, and even emotionally, for many – became the vaccines.Mr.Gates articulated what became our master narrative: Public health would stop the spread with extemporizing measures such as lockdowns, discouraging social functions and travel, and closing schools and businesses until the vaccines arrived, all of which would protect us until we achieved vaccine-induced herd immunity everywhere, which, we were told, would eliminate the virus.We put our faith in the vaccines, while other approaches – such as drugs for early treatment, or a role for our natural immunity, or lowering our personal risk factors, for instance – got comparatively less attention.
Key individuals predicted – half promised, really – we’d be done with COVID, at least in the West, by the summer of 2021.In February, 2021, Pfizer’s CEO, Albert Bourla, said the vaccine was still offering strong protection at the six-month mark and “indicators right now … are telling us that there is a protection against the transmission of the disease.” That April, Dr.
Ugur Sahin, the CEO of BioNTech (which developed the vaccine for Pfizer), told reporters , “Europe will reach herd immunity in July, latest by August.” It wasn’t a tough sell.Who would not want it to be true? Having no pandemic experience, we took them at their word.
Politicians fostered the idea that our proper aim for handling COVID would be to “eliminate it everywhere,” as Prime Minister Justin Trudeau said .Early treatment doesn’t promise that, though it might lower death rates.Eradication had more psychological appeal: let’s get it out of our lives forever.
Yet, in dismal December, 2021, two years in, with cases soon to reach record highs, and another lockdown looming and vaccines waning, it wasn’t working out that way.Perhaps if we hadn’t been so focused on one tool things might have gone differently.And perhaps if certain voices hadn’t been silenced, and others handed a megaphone, our pandemic tool kit, and mindset, would have been different too.
People applaud health-care workers from their balconies on the second day of France’s first pandemic-related lockdown in Paris, 2020.Paris is home to a psychiatric hospital where COVID-19 questions raised theories about the antiviral properties of antidepressants.THOMAS COEX/AFP via Getty Images
Early in the pandemic, at the Sainte-Anne site of the Parisian mental hospital, Psychiatrie & Neurosciences, something mysterious occurred.The staff started contracting COVID in high numbers, but their patients, gravely mentally ill, did not.
Three staff got COVID for every patient, despite the patients having more risk factors, such as being overweight, or having cardiovascular disease.
Someone wondered, could it be that the patients’ psychiatric medications were protecting them? The staff homed in on chlorpromazine, a common antipsychotic medication, and learned it had antiviral properties against SARS-Cov-1 and MERS-CoV (the predecessors to SARS-CoV-2).In a May, 2020, publication , they proposed repurposing it for treating COVID-19.
French psychiatrists and scientists next did a multicentre study , looking at 7,230 patients who had been hospitalized in Paris for severe COVID-19.Coincidentally, 300 of the patients were taking antidepressants.The data showed that those on Selective Serotonin Uptake Inhibitors (SSRI) – a kind of antidepressant – were less likely to require intubation or die.Not all SSRIs worked equally, but those that did reduced major inflammatory problems (the COVID “cytokine storm” that often kills).Lab research showed that the SSRI fluvoxamine had an antiviral effect, and a salutary effect on blood platelets that might protect patients from blood clots.
A sample of SARS-CoV-2, the virus that causes COVID-19.NIAID-RML via AP
Meanwhile, back in the U.S., in parallel process, a child psychiatrist, Dr.Angela Reirson, caught COVID in early 2020.
Sick at home, she started doing research.She recalled a study on mice she had read the previous year.The mice had sepsis – a dangerous response to infection that can kill .
Something akin to sepsis can happen in serious COVID.In the 2019 study, mice with sepsis were given fluvoxamine, which halted the condition.So, in March, 2020, Dr.Reirson contacted another psychiatrist, Eric Lenze, a colleague of hers at Washington University in St.Louis.Dr.Lenze was a specialist in repurposing drugs.
Realizing fluvoxamine had a great safety record, he launched its first small randomized control trial of COVID patients.Not one of the 80 volunteers who got fluvoxamine deteriorated or got COVID lung damage, whereas 8 per cent of the 72 who got a placebo did deteriorate.The findings were published in JAMA in November, 2020 .
Next came the Together Trial , the world’s largest placebo study of COVID drugs, co-led by McMaster researcher Edward Mills and Brazilian physician Gilmar Reis.To do large trials you need a lot of cases, and Brazil had two million.The study was published Oct.27, 2021, in the Lancet.
It studied about 1,500 unvaccinated patients with COVID-19 who also had another serious illness and were at high risk for hospitalization.
Half were given fluvoxamine, half a placebo.In those who took the fluvoxamine as prescribed it reduced the odds of hospitalization or emergency care by 66 per cent and death by 90 per cent.
Ontario Premier Doug Ford and government officials give a news conference in 2020 about the pandemic.Nathan Denette/The Canadian Press
The Ontario Science Table noticed these findings and on Dec.20 it put fluvoxamine in the guidelines, for doctors to prescribe on an outpatient basis if needed, recognizing “the need for outpatient treatment options with a reasonable safety profile during an anticipated spike in COVID-19 cases due to the Omicron variant.”
That was significant, because early treatment of COVID – measures we can take to avoid symptomatic cases from worsening, requiring hospitalization – has been so minimal.In Ontario, treatment includes monoclonal antibodies ( now only one works with Omicron ) for specific people at risk, and steroids.
Otherwise outpatients were told to rest, drink fluids, and hope their immune system would handle the virus.
True, there was much talk of brand-new, non-repurposed drugs for early treatment.Pfizer’s Paxlovid, just approved by Health Canada on Monday, is very new.
But repurposed drugs have a track record , and thus often a safety advantage.And the generic ones are cheap.Fluvoxamine costs about $15 for a course of treatment.Repurposed drugs are used by poorer countries that can’t afford vaccines or expensive early treatment drugs such as Paxlovid ($500) or Molnupiravir (US$700 and not yet approved in Canada).
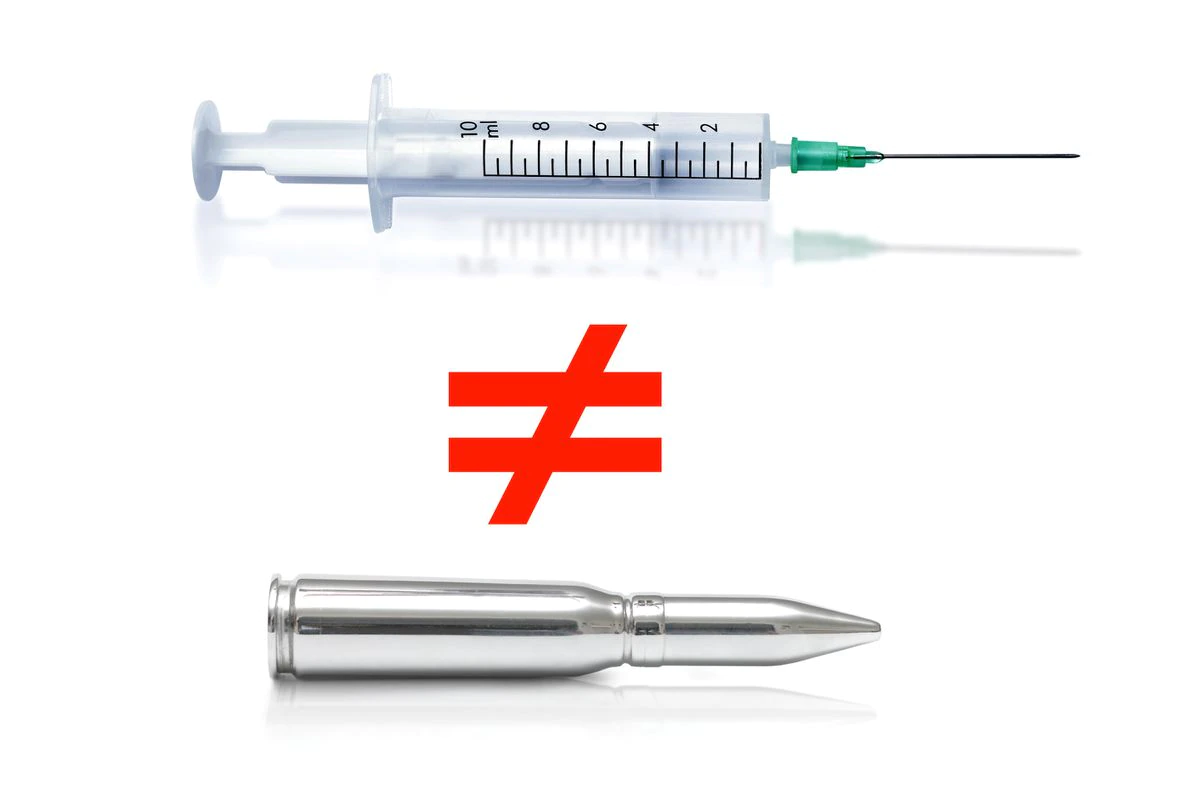
So why hasn’t treatment focused more on repurposed drugs?
First, because the master narrative, once it took hold, directed our attention away from this possibility.
Second, in North America, the first repurposed drug that came to public attention was hydroxychloroquine.When it was endorsed by then-president Donald Trump it became highly politicized.People’s opinions about it often had more to do with their political affiliation than whether they had read any of the (now) 303 studies.Third, agencies that regulate drugs, such as the U.S.Food and Drug Administration and Health Canada, mandate that any drug they evaluate have a sponsor, usually a drug company agreeing to assume liabilities for the drug.It’s an extremely expensive process.
If an old, cheap generic drug shows promise for repurposing, it still needs a sponsor to get approved for that.But drug companies have no financial incentive to do so.So usually there are no sponsors, and the drugs languish.
A person walks past a mural honouring health-care workers in Toronto.Imagery of war and communal struggle became a big part of the COVID-19 narrative: This mural, for instance, uses the pose and bandana of Rosie the Riveter, a Second World War icon.
Nathan Denette/The Canadian Press
Of all the reasons that we didn’t focus on repurposed drugs, I would argue, the master narrative was the most important, because of the way it organized so many people’s thoughts, attention and emotions.
The narrative would not have been nearly as problematic had it not been so tied into something else: the military metaphor that has defined our COVID experience from the beginning.This master narrative was our battle plan and this was a “war” to eradicate the enemy virus.
This military metaphor seems second nature in medicine.We are always in a “war against cancer,” or “combatting” heart disease, Alzheimer’s, and AIDS.But this way of thinking only became common in medicine several hundred years ago, after the philosopher Francis Bacon argued the goal of science should change from what it had been – “the study of nature” – to the very practical “conquest of nature.” Soon physicians were speaking of “conquering” disease, with “magic bullets.” We increasingly left behind the original Hippocratic mindset of medicine as an extension of nature, which involved working with it, as an ally, wherever possible – not to conquer, but to heal, often with the help of the patient’s own healing capacities.
Scientists were to be soldiers in this new army.And here a problem arose.Despite some similarities, science (and medicine) is really best not construed as warfare – and the kind of virtues that may suit soldiers in an army (following an authority without questioning), are vices in science, which is a mode of critical inquiry.Modern science arose because the world was filled with too many dogmas and orthodoxies that were not to be questioned.
That is why the motto of the Royal Society, the first national scientific institution, became Nullias in verba , “Take Nobody’s Word For It.” It’s the role of scientists, as Nobel Prize-winning physicist Richard Feynman said , to question the experts, and fellow scientists, and debate each experimenter’s conclusions, which are based on human judgments and interpretations of data, until there is certainty the conclusion can resist all onslaughts.
Reappraisal of any prevailing narrative requires taking in new insights, which, by definition, arise from a minority viewpoint.
When a military metaphor sweeps through a society or a bureaucracy beset by fear, all-or-nothing, you-are-with-us-or-against-us thinking follows.We become more prone to see someone who doesn’t go along with the majority view – including scientists who spot problems with the reigning narrative – as putting the rest of us at risk, and a “traitor,” rather than as someone doing their job.They are attacked, censored or self-censor to survive.In war, you shut up and follow orders, or get court-martialed.
We are especially suspicious of other people during contagion, because our brains are fired up by a primitive circuit that protects us by making us obsessively preoccupied with the purity of those around us.Will this person get me sick? It even fires if we think their actions, or even policy proposals might be risky.The circuit, called the behavioural immune system , causes us to fear, loathe and feel rage toward the “impure” germ bearer.
It results in many false alarms (think of someone driving alone with a mask on).It’s one reason debates about vaccines are emotionally radioactive.Some vaccinated people feel all the unvaccinated bear germs, while some unvaccinated people feel vaccine may put germs or toxins in their bodies.
A nurse administers a COVID-19 vaccine in Orange, Calif., this past summer.Jae C.Hong/The Associated Press
This past summer , as news broke that there were breakthrough infections and vaccine protection against infection was waning, the North American media began to advise us to lower our expectations for them: “Vaccines Can Only Do So Much,” read a headline in The Washington Post.Many readers were caught completely off guard.
In part they were surprised, because the censorship of scientists who held dissenting views – and had been warning this might happen – was much more widespread than many are aware of.
According to an Amnesty International report published in October, censorship and harassment of health professionals, and others, has been a problem “across the world,” during the pandemic.Most singled out are those who express critical opinions of their governments’ policies (e.g.restrictions of movement, lockdown, or criticisms of government dispensing with civil liberties).
The censors justified these actions as simply banning “misinformation” and “prevent[ing] panic.” In North America people were not imprisoned, but many brilliant scientists and physicians with proper credentials from places such as Harvard, Oxford and Stanford, were under fire .Physicians were vilified for questioning government policies on lockdowns, masks, aspects of vaccines, mitigation or unproven treatments – the very things that were, of course, the subject of serious continuing scientific debate.In some jurisdictions in North America physicians are threatened by their regulating boards with suspension or revocation of their medical licenses for spreading “misinformation,” forcing some doctors to have to choose between what they – rightly or wrongly – see as their patient’s best interests, and their own livelihood.
But as the Amnesty report states, “Winning the battle against the virus includes not just government led actions and top-down diktats, but also bottom-up approaches which can only come about if the rights to freedom of expression and access to information are fully enabled.”
Warning signs are seen at a COVID-19 testing lab in Ingelheim, Germany.
Kai Pfaffenbach/Reuters
There were “snake oil” claims on the internet, yes, but generally when scientists and health care workers were party to these quarrels, it was because there was a scientific debate.In such a case, to accuse one’s opponent of spreading “misinformation” is to pre-emptively ascribe to oneself an unjustified certainty – and to one’s opponent bad faith.At times no one really knew what was more harmful – e.g.keeping children out of school, or sending them in.
There was incorrect information aplenty in our novel situation, and that included some spread by officials who flip-flopped multiple times on masks, or who, claiming to “follow the science,” differed with officials in similar jurisdictions, based on changing data.
This, in medicine, is called the problem of “medical reversal.” An approach thought to be helpful is proven to be harmful, and vice versa.Sometimes two studies can contradict each other even on the same day.Physician-scientist Vinayak Prasad , of UC San Francisco, argues it is the most important problem facing medicine today.The problem of medical reversals didn’t disappear the day the virus landed on our shores.
We had not only a virus problem, but a medical reversal problem.
The medical boards were in an unusual situation, torn between once-cherished traditions of scientific debate, and the atmosphere of crisis and their wish to do their part in “the war.” After all, it is vital that public health, and its officials, in a crisis, be able to convey consistent messages as they ask citizens to change their behaviours, and undergo various privations.But if those messages are to be persuasive, and the requests for such privations scientifically arguable and legitimate, the actions must be based on a full, open, unhampered scientific process solid enough to withstand scientific criticism and debate.Why else should the public go along? Censorship, by giving the public the false impression there are no medical controversies, undermines the censor’s own claim to speak in the name of science and public safety.Ironically, it guarantees the public will be left misinformed.
People light a display of about 1,500 candles in memory of COVID-19 victims in Greifswald, Germany.
After the original virus spread around the world, more contagious variants like Delta and Omicron superseded it, and researchers scrambled to understand how effective vaccines would be against them.Stefan Sauer/dpa via AP
The authors of the master narrative tend to say the main reason that things have not gone as they predicted is because variants arose.But if anything could have been predicted, it is that viruses mutate.Columbia virologist Vincent Racaniello described how fellow scientists were worried that the new mRNA technology, by focusing on only a small portion of the virus, the spike protein, would make it easy for the virus to “get around” or escape the vaccine through mutations.“That’s partly why,” he said in May , “all the variants are arising now, because we have only the spike epitopes in there.” That view didn’t get much of a hearing.
It wasn’t just the variants’ role in declining vaccine efficacy that surprised people.There was something about the execution of the original clinical trials, conducted by the pharma companies themselves, on their own products that also led to this surprise.
It’s worth going back for a moment and looking at how the problem unfolded.
In December, 2020, the new mRNA vaccines were rolled out, and were, according to the randomized clinical trials, 95 per cent (Pfizer) and 94.5 per cent (Moderna) efficacious in stopping infection.Physician-scientist Eric Topol, head of Scripps Labs, said these vaccines “will go down in history as one of science and medical research’s greatest achievements.”
But by the time summer 2021 arrived, real world experience contradicted Mr.
Bourla’s and Dr.Sahin’s claims of potency at six months, no transmission by the vaccinated, and imminent herd immunity.Pfizer’s Mr.
Bourla, in his February interview, had called Israel “the world’s lab,” because it was vaccinated with the Pfizer extensively and several months ahead of other countries, giving the world a glimpse of its future.
But when Israeli public health released its six-month data, they showed that vaccine effectiveness had dropped to 39 per cent, and Delta was surging.(The FDA had originally said it would not approve a vaccine less than 50-per-cent effective.) A Mayo clinic study showed that after six months, protection granted by the two Pfizer doses dropped from the original 95 per cent to 42 per cent.Another Israeli study showed it had dropped to 16 per cent .That huge discrepancy couldn’t be attributed just to the new variant, Delta, because protection was already fading at five months for the earlier variants too .
Pfizer doses are prepared at a temporary vaccination centre in London.DANIEL LEAL/AFP via Getty Images
So why such a discrepancy? The original studies were clinical trials.The Pfizer study followed about 38,000 people without COVID who were divided in two groups – half got the vaccine, and half a placebo.
The investigators asked the question: could the vaccines prevent symptomatic cases of COVID-19? But, as Peter Doshi, senior editor at the British Medical Journal, warned , “None of the trials currently under way are designed to detect a reduction in any serious outcome such as hospital admissions, use of intensive care, or deaths.” He explained that, “Because most people with symptomatic COVID-19 experience only mild symptoms, even trials involving 30,000 or more patients would turn up relatively few cases of severe disease.” Susanne Hodgson of the University of Oxford agreed : “The current [randomized control trials] that are ongoing are … not powered to assess efficacy against hospital admission and death.”
The Moderna report to the FDA on Dec.17, 2020, confirmed “there were no deaths due to COVID-19 at the time of the interim analysis to enable an assessment of vaccine efficacy against death due to COVID-19.” Moderna followed about 30,000 people.When asked by the British Medical Journal, why the trial had not been designed to assess if the vaccine could prevent hospitalization and death, Moderna answered : “You would need a trial that is either 5 or 10 times larger or you’d need a trial that is 5-10 times longer to collect those events.” In the Pfizer study of 38,000 people, not a single person in the placebo or the vaccine group died of COVID.By publication date, only one person had died of COVID in the Moderna study.
To state it clearly: One person out of about 70,000 in the combined studies of Pfizer and Moderna actually died of COVID.In the real world, at the time, about 60 per cent of COVID deaths were in people over 75 years of age.
But only 4.4 per cent of that age group were in the Pfizer study.The sample chosen was not appropriate to answer the public’s most pressing question: Could the vaccines save lives?
And how long had the Moderna and Pfizer vaccines been studied, when released for mass use in the winter of 2021? Two months.
These studies looked at the vaccines at their most potent, in a low risk population, and gave us a flattering snapshot.But COVID-19 is a movie.
In contrast, the Mayo study, and the Israeli data, were looking at data over a more realistic time course to test effectiveness.
The waning created a crisis in Israel.
Dr.Sharon Alroy-Preis, director of Israel’s Public Health Services, told the FDA Vaccine Advisory Committee on boosters, why the country became the first to roll out a third shot: “ What we saw prior to our booster campaign was that 60 per cent of people in severe and critical condition were immunized, doubly immunized, fully vaccinated and as I said, 45 per cent of the people who died in the fourth wave were doubly vaccinated.” Most “breakthrough infections” are indeed mild, but she was describing life-threatening ones in the vaccinated.As breakthrough infections became commonplace throughout the world, noted Harvard epidemiologist Michael Mina said , the message that “this is only an epidemic of the unvaccinated … is falling flat.”
A newly vaccinated patient takes a selfie with the nurse at the Sheba Medical Center in Ramat Gan, Israel.Tsafrir Abayov/The Associated Press
As for Dr.Sahin’s claim that we were on the brink of vaccine-induced herd immunity and being rid of COVID altogether, experts such as Larry Brilliant (who had helped eradicate smallpox with vaccines) and five other scientists wrote in Foreign Affairs in July, 2021, “Among humans, global herd immunity, once promoted as a singular solution, is unreachable .” They explained in precise detail why COVID-19 was unlike smallpox, and it could not be “eradicated,” such as the fact it is growing in a dozen animal species already.
“If we are forced to choose a vaccine that gives only one year of protection,” said Dr.Brilliant , “then we are doomed to have COVID become endemic, an infection that is always with us …” That vaccines would get us to a vaccine-based herd immunity had been one of the two main scientific justifications for vaccine mandates.Now it was gone.
The other justification for mandates had been that the vaccinated don’t transmit the virus.
Most of us had presumed, when we got our first doses, that we couldn’t pass the virus on to others.Public statements repeatedly praised people for “doing your part to stop the spread.” But in August, CDC director Rochelle Walensky told CNN , when asked why the vaccinated must wear masks, “Our vaccines are working exceptionally well.They continue to work well for Delta; with regard to severe illness and death, they prevent it.
But what they can’t do any more is prevent transmission.”
In fact, the original randomized clinical trials for Pfizer and Moderna did not test if the vaccines stop transmission.Now our best hope was that the vaccinated might transmit less than the unvaccinated.Several studies could be interpreted as showing this.
But others found the vaccinated likely had equal transmission.One study , conducted in a prison , concluded that the vaccinated prisoners had as much “transmission potential” as the unvaccinated prisoners, adding, “clinicians and public health practitioners should consider vaccinated persons who become infected with SARS-CoV-2 to be no less infectious than unvaccinated persons.” Dr.Cyrille Cohen, head of the immunotherapy lab at Bar-Ilan University, and adviser to the Israeli government on vaccine trials, said that with respect to transmission with Omicron, “we don’t see virtually any difference … between people vaccinated and nonvaccinated,” adding “both get infected with the virus, more or less at the same pace.The rancour that we, the vaccinated, are increasingly directing against the unvaccinated, fuels itself by remaining wilfully oblivious of this later painful truth: we too spread, to ourselves, and to the unvaccinated, as they to us and each other.”
The master narrative was silent about natural immunity and its relationship to vaccination status.
Many scientist-physicians, from prominent universities in the U.S.with specialties in public health, argue that one can be for the use of the COVID vaccine, but also against mandating it for unvaccinated people who are already immune.
These scientists maintain what matters is not whether a person is vaccinated or not, but whether they are immune or not.Thus, the European Union recognizes natural immunity in its Digital COVID Certificate , which is in lieu of a vaccine passport, and is not limited to proof of vaccination.You could get a passport and travel if you have been vaccinated or if you have “recovered from COVID-19″ or if you have a recent test saying you are negative.
For air and train travel , Canada has also acknowledged recovery from COVID as an exemption, if one presents a recent negative test – but, inconsistently, natural immunity is not recognized in most other quasi-mandate situations here.Such scientists think it irrational that government calls for mass mandates are escalating just as the core original justifications for them – that the vaccinated don’t transmit the virus, and the vaccine will bring us to herd immunity – have collapsed.
A mobile phone shows a European Union digital vaccine certificate.OLIVIER MORIN/AFP via Getty Images
Those unvaccinated people who were exposed to the virus, make up a huge number.For instance, in the U.S., according to a Columbia University study , by Jan.
31, 2021 (before many vaccines had been given) 10 months into the pandemic, 120 million Americans had natural immunity.
Now, 12 months later, with the much more infectious Delta and Omicron variants, it is likely a highly significant majority of the unvaccinated now have natural immunity.
A recent pivotal study from South Africa – not yet peer reviewed – shows that in poor communities, where there was modest vaccination (39 per cent of adults), more than 70 per cent of people had already been exposed to the virus in previous waves, going into Omicron.The twice vaccinated had more protection than those who were unvaccinated and never had COVID.But the unvaccinated who had COVID and recovered had more protection from severe disease than the vaccinated.One Israeli study showed that the unvaccinated who recovered from COVID have 27 times less risk of reinfection compared with the vaccinated, and nine times less risk of hospitalization.
In a recent Munk Debate , Harvard’s Dr.Martin Kulldorff, an epidemiologist and vaccine safety specialist, argued that mandating vaccines for the naturally immune “actually creates problems because when people see that they are forced to take a vaccine that they don’t need because they already are immune, that causes a lot of distrust in public health.And we have seen during this last year and a half that all the hard work we’ve done over many decades to build trust in vaccines is now disappearing because we’re making these mandates that make no sense from a scientific or public health perspective.”
Public health moves at the speed of trust, as physician Rishi Manchanda wrote.Of the two main approaches to public health – the participatory, and the coercive – the coercive usually makes enemies, and tears society apart.
It’s like a hare: it has quick victories.The participatory approach, is a tortoise; when it fails to persuade, instead of blaming those it serves, it asks, as a scientist might, where have I fallen short, and aims to do better.
People are seen through a frame that reads ‘third dose reinforcement’ at a mass vaccination clinic for people over 60, in Mexico City.Third doses proved very effective against Delta, and are still important at preventing hospitalization and death in Omicron cases.Luis Cortes/Reuters
Israel’s third booster helped beat back the Delta wave.Then Omicron hit.On Dec.19, The New York Times headlined an article , “Most of the World’s Vaccines Likely Won’t Prevent Infection from Omicron.” Thankfully, the vaccines still seemed like they would prevent those infections from becoming severe – the key point.A Kaiser study showed that two doses, over time, fell to zero efficacy against Omicron.
Then Danish data showed that a booster offered protection against severe disease, but “only to those over 70 years.” But would boosters wane too? The U.K.Health Security Agency study showed the protection from the Pfizer booster (third shot) had dropped to 45-per-cent coverage at only 10 weeks.
Then on Jan.1, 2022, a study of vaccine effectiveness against getting infection in Ontario – not yet peer-reviewed – showed a trend that had already shown up in Denmark.It examined provincial data and was authored by members of Public Health Ontario, ICES, the Dalla Lana School of Public Health, UHN, and other major Ontario university and health programs.
They found two things of note.
The first was that “VE [vaccine effectiveness against getting infection] against Omicron was only 37% > 7 days following a third dose.” That doesn’t mean that those in the other 63 per cent who did get the infection might not have got some protection from severe infection, but the authors were unable to measure protection from severity from the data that had.
The second finding was more dramatic:, “We also observed negative VE against Omicron among those who had received 2 doses compared to unvaccinated individuals.” Translation: Negative VE means that the vaccinated got more infections than the unvaccinated.
That “negative finding” they noted, had already been observed elsewhere.“In the Danish study , there was no significant protection against Omicron infection beyond 31 days” after the second dose of the Pfizer.The Danes also found significant negative VE estimates 91-150 days after the second dose.” The Danish study showed those vaccinated with the Pfizer had a 76.5 per cent greater chance of getting infected than unvaccinated people.With the Moderna, the vaccinated had a 36.7 per cent greater chance of getting infected than the unvaccinated after 90 days.
The authors discuss how negative vaccine effectiveness finding might arise.It may not mean that the vaccine actually decreases the person’s immunity.There could be confounding factors.
One possible explanation they raise is that in Ontario, a vaccine certificate system was introduced in the fall of 2021, and only those who had two doses could travel by air, rail, go to bars, gyms, etc., and so they may have had more social contacts than the unvaccinated who were shut in.But even if true it would still mean that the vaccines are not protecting us as much as we’d like, which is nothing to celebrate.
Another possible explanation the authors raise is “the possibility that antigenic imprinting could impact the immune response to Omicron.” It had been observed in the past that the immune system is highly influenced by the first exposure to a microbe (antigen) that it encounters.It’s called “original antigenic sin.” When a second exposure occurs, to a similar but not identical microbe, the immune system reacts as though it is targeting the original microbe.
But the new invader isn’t the original, and so the immune system is actually less effective in dealing with this.In essence the immune system is weakened for a microbe too similar to its first similar exposure.This phenomenon was originally described as occurring in influenza on occasion.
This is only a theoretical possibility here, not proven for COVID, but now a matter of scientific discussion .The negative vaccine efficacy has since shown up in Iceland , and the U.K.as well.The Ontario authors are to be applauded for thoughtfully laying out some possibilities to think through, so as to determine what might be the cause.
A COVID-19 mural in Vancouver urges people not to worry.Jonathan Hayward/The Canadian Press
We’ve had so many mood swings.We had been through a year of defining vaccine success as eliminating the virus, then as lowering infection and stopping the spread, to discovering there were breakthrough infections and transmission to other people, but that they still lowered our risk of hospitalization and death – that’s worth a lot – though not always in the most vulnerable.
In the West, many have responded to waning vaccine protection with time by doubling down, proposing ever more boosters.What is the scientific evidence for frequent boosters? That’s a matter of scientific debate.
The original Pfizer study submitted to the FDA booster meeting was shockingly tiny – a mere 306 patients were given the section, and they had been followed for only a month, and, again, most of the subjects were younger than those at risk (18-55).Pfizer wanted it on that basis rolled out to millions.That was enough to get FDA officials asking hard questions.Crucially, nobody had studied the long-term effects of multiple mRNA boosters – there hasn’t been time.The FDA refused Pfizer’s recommendation to approve the booster for the entire U.S.
population, with the top two heads of its Vaccine Research and Review Committee, Dr.
Marion Gruber, (the head, and former acting chief scientist at the FDA), and Philip Krause (deputy director), and international colleagues, writing in the Lancet:
“ There could be risks if boosters are widely introduced too soon, or too frequently, especially with vaccines that can have immune-mediated side-effects (such as myocarditis, which is more common after the second dose of some mRNA vaccines, or Guillain-Barre syndrome, which has been associated with adenovirus-vectored COVID-19 vaccines [like the AstraZeneca or Johnson & Johnson]).If unnecessary boosting causes significant adverse reactions, there could be implications for vaccine acceptance that go beyond COVID-19 vaccines.”
When the head scientists of the FDA Vaccine Review committee and colleagues raise such questions, it can’t be dismissed as fringe fear-mongering.Shortly after, Dr.
Gruber and Dr.Krause quit the FDA because the Biden administration was putting pressure on them to approve boosters before the vaccine committee had even met.The standard practice for approval is for the agencies to convene panels of outside experts to review the data openly, weigh risks and benefits, and take votes.But in December, the FDA and CDC leadership three times took the extraordinary step of not convening those experts for key booster meetings, in essence going around them because committee members had warned that the science supporting boosters for younger people was weak to non-existent, and they had safety concerns.Dr.Paul Offit, perhaps the most high profile provaccine physician-scientist in America, who was on the FDA panel told The Atlantic , he wouldn’t advise a booster for his healthy son in his 20s, or a healthy male in his teens, because the risks of myocarditis (higher in males) outweigh the benefits.Dr.Offit rejects the CDC’s and FDA’s all-or-nothing approach to children’s vaccination.
Vinayak Prasad, the UCSF epidemiologist, says if you put the Danish, Ontario, U.S., and Kaiser studies about Omicron together, “it’s time to face the reality about the vaccines.”
“ Two doses of vaccine does nothing or almost nothing to stop symptomatic SARS-CoV-2,” he says.
“Three doses barely does anything, and the effect will likely attenuate over time.” He says, “Booster mandates make no sense.… Boosting should happen in populations where it further reduces severe disease and death – a.k.a.older and vulnerable people.”
With Omicron surging, Israeli public health met to discuss a fourth booster.The New York Times reported that some scientists on the Israeli government booster advisory panel, “warned that the plan could backfire, because too many shots might cause a sort of immune system fatigue, compromising the body’s ability to fight the coronavirus.” This immune system fatigue was, perhaps, not inconsistent with negative vaccine efficacy.
It’s not proven, but the fact that public-health officials were voicing such concerns shows that the doubling down strategy on boosters is being reappraised on safety lines.The EU, in a reversal, has just come out against regular, continuing boosters, saying they are afraid it will weaken the immune system ..